It's been a full year since I last posted! I'll have to go back to that one and see what needs to be updated since we've learned so much about severe acute respiratory syndrome coronavirus 2, or SARS-CoV-2, the virus that causes coronavirus disease 2019 (COVID-19). That's for another day, but I'll give you one comparison. At 3:08pm on March 15th, 2020 there were 162,687 cases of COVID-19 reported around the world, according to a dashboard created by the Johns Hopkins Centers for Systems Science and Engineering. At 11:28am on March 28th, 2021 there were 126,911,173 reported cases globally. That is staggering and, by all accounts, a gross underestimate. Remember the iceberg analogy. People who either don't get sick or only feel a little sick are far less likely to be tested, even during a pandemic, so we don't have the whole picture.
The virus is still circulating in our communities
and it isn’t going to just magically disappear any time soon. It's still infecting
people at high rates and it's mutating, or changing, to become a better virus.
To be the best virus you can be is to spread rapidly and keep your host alive so they
can sneeze and cough and send you out into the world to infect another. Humans
are working hard to find ways to slow down the spread and to keep people from
getting severely ill or dying. It's been one year since the World Health
Organization declared a pandemic. One year and we've got vaccines people! This
is AMAZING. The best way to protect yourself from getting extremely sick with
COVID-19 and needing to be hospitalized, or from dying, is to get vaccinated.
If you don't want to listen to me, listen to Dolly Parton. https://www.youtube.com/watch?v=BjfT6H6QUIA.
Continue to avoid getting infected until you can get vaccinated. Keep wearing
your masks, stop swapping air, wash your hands. You know the drill.
There are three vaccines available right now in the United States. Do you know how they work? <Looks furtively left, then right. Leans in and whispers> I don't really know either. Let's find out together! Full disclosure: I am not a vaccine specialist, nor do I have any deep understanding of the immune system. Immunology, the study of the immune system and immune response, is super complicated. Like I don't even have the right words complicated. Like actual immunologists, the doctors and researchers who study immunity, say it's complicated to them. The descriptions you're going to read of immune responses to these vaccines are very high level and not in any way certain of what will actually happen in your body or my body or your neighbor's body. Let's learn anyway!
The virus and disease.
Before we get started talking about vaccines, let's learn about the virus and the disease it causes. In terms of microbes, SARS-CoV-2 isn't very complicated. From the outside in, there are protein spikes on the outer layer of a fat coat that is protecting a single strand of RNA, or ribonucleic acid. You've heard of DNA, right? The double helix? The double-stranded stuff that contains all of the genetic information that makes you, you? Well, RNA is a single strand of the same type of genetic information. SARS-CoV-2 RNA contains the codes for how to make more virions. Virions are individual viral particles.
The protein spikes on the outer surface of the virus attach to receptors in your body called ACE2. These receptors are found on nearly every type of cell in your body (nose, lung, heart, kidney, brain, intestines) which is why we see symptoms ranging from common cold-like symptoms to loss of taste and smell all the way to organ failure. The viral particle spike attaches to an ACE2 receptor, enters the cell, trades out the cell's plans for its own, sits back with a cocktail and a smoke and watches the world burn.
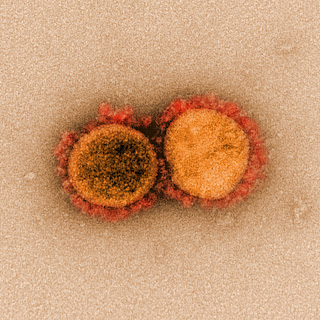
Okay, not quite, the virus isn't a sentient being. Once the virus spikes have attached to the ACE2 receptors, the virus' fat coat fuses with the outer surface of the human cell and the RNA is released. Inside the cell, the RNA bumps into a ribosome. Ribosomes are the protein-making machinery of a cell. The ribosome reads the genetic information of the RNA strand like a blueprint and begins to make the parts of the virus - spikes, fat coats, some proteins, and more RNA. Then those parts are put into a little factory and transport system called the Golgi apparatus which assembles the parts into new individual virions, packages them, and sends them out of the cell. And so it goes; RNA becomes parts, the parts are assembled, and new virions are released. After time, virus overwhelms the cell and the cell self-destructs. All of the remaining virions are released into the body where they seek out ACE2 receptors on new cells or are picked up by respiratory droplets and leave out the nose and mouth. The process is exponential, meaning that one viral particle can result in hundreds of additional particles. Each of those go on to make hundreds more and they can quickly take over thousands of cells in your body, creating millions of virions. The image below is from a fancy microscope called an electron microscope. It is used to capture clear, multidimensional images of very tiny things like viruses. This is an image of a cell during death. The green parts are the cell and the little bumpy purple balls are SARS-CoV-2. One cell and hundreds of viral particles.
 |
| Image credit: NIAID-RML |
For any of that to happen, you have to first be exposed to the virus. You are exposed by coming into contact with respiratory droplets containing viral particles. The viral particles enter your body through mucus membranes like your nose, mouth, and eyes. We know close contact with infectious respiratory droplets is still the most common way to be exposed. Close contact is described as within six feet which is approximately the distance that large respiratory droplets travel before dropping to the ground or other surfaces. The virus can be carried in much smaller droplets called aerosols that travel farther distances and hang in the air longer. So is it airborne? There is a lot of debate going on in the science and health care world about this very topic and I'm not going to pretend like I completely understand it. Viral particles travel in respiratory droplets. Large respiratory droplets hold more viral particles than small ones. Large droplets fall to the ground (or other surfaces) faster than small ones; that's just physics. Small droplets are suspended in the air and can travel farther distances. They also dry out faster, leaving the virus vulnerable. The fat coat will no longer protect the RNA inside and once exposed, the RNA starts to break down. In terms of infectious diseases, airborne refers to the route of transmission. Not just that the virus is in the air but is it infectious. Can it cause infection?
Documented cases of airborne transmission have occurred under specific circumstances. Studies of these transmission events have concluded that airborne transmission is more likely to occur in situations involving enclosed spaces, spaces with poor ventilation, and instances of prolonged exposure to respiratory droplets. Like choir practice, exercise class in a room at the gym, or spending time with family in a poorly ventilated home. In looking at how SARS-CoV-2 has spread in these specific settings and also generally, evidence still supports that the majority of transmission is by large droplets. Masks, distance, and handwashing are still the best ways slow the spread of the virus.
Reflecting back to early on in the pandemic, I didn't think we should all wear masks. When we only had the options of surgical masks and N95s, I discouraged people from trying to purchase them for fear that our health care workers wouldn't have enough. I was worried that even if they had masks, people wouldn't wear them correctly and would inadvertently infect themselves. I know I'm not wrong about that because I see y'all out there in the grocery store with your nose hanging out of your mask.
Come on. Your nose is part of your respiratory system and you gotta cover that up. Nobody wants to see your nose. In terms of availability of masks, I could never have imagined all the Etsy shops, sewing circles, and small and large businesses that got into the mask-making game. I was flabbergasted. Many research studies have been conducted to learn more about how masks can help keep our large respiratory droplets closer to us and away from others. This is referred to as source control. Surgical-type masks, double or triple layer cloth masks, and other layered face coverings work by trapping larger respiratory droplets that may contain lots of virus. Masks that work for infection control are the kind like N95 masks. They must fit properly so that they create a seal around your nose and mouth and are made of material that filters out very tiny particles. Those are the kinds of masks that should be worn by health care workers who are treating patients with COVID-19. Your cloth mask can somewhat help keep you from becoming infected by trapping large droplets that you may come into contact with when you're close to someone who is infected. Masks aren't magical, they're just one part of how we can prevent transmission. Keep distance and wash your hands frequently too!
Alright, back to the learning. You can be exposed to SARS-CoV-2 virus, but not become infected. Suppose a small amount of virus gets into your body and either cannot find any ACE2 receptors or is trapped in the mucus and hair in your nose or are spotted immediately by an alert immune cell and are killed. No infection.
Now let's say the viral particles did find ACE2 receptors and have entered at least some of your body's cells. Your cells are infected! You can be infected and not have any symptoms of the disease COVID-19; you don't feel sick. This is referred to as asymptomatic infection, or without symptoms. The virus is being replicated in your cells, but your body is not sending out alerts to raise your temperature or cause inflammation. Understand that asymptomatic is in the eye of the beholder. This is often determined by asking someone if they have symptoms or had symptoms. Humans are notoriously really bad at doing health self-assessments. Do you remember how you felt three days ago? I don't. I can barely remember what I felt like an hour ago. There's also the caveat that many people who are not feeling any symptoms at the time of testing actually do go on to feel sick a day or three later. If nobody follows up with them, we never know that they did have symptoms. In some studies, these individuals are included in the overall asymptomatic number when they were actually presymptomatic, meaning they tested positive before symptoms started. People who are asymptomatic or presymptomatic are likely major drivers of transmission during the pandemic because they feel fine and go to work or hang out with friends or go to the gym all the while spreading a lot of virus around, unknowingly. Asymptomatic and presymptomatic infections are why we ask you to wear a mask and keep distance even if you're feeling fine.
If you have been exposed to and infected by the virus, you may
come down with symptoms of COVID-19. It can take two days up to two weeks after
being exposed before you begin to feel sick, but most symptoms start around day 4 or 5. The viral particles have taken
over many cells in your body and your immune system has mounted a defense. A
lot of symptoms of illness are actually related to the fight against the virus, symptoms like fever, body aches, and tiredness. Other symptoms come about
because of the cell damage caused by the virus. If the virus has infected
certain cells in your neurological system, you may lose your sense of taste and
smell. Still other virus infects the cells of your blood vessels and you may
develop clots that can lead to stroke or your heart may begin to malfunction.
Remember earlier when I said that ACE2 receptors are found on nearly every cell
type in your body? This is why people with COVID-19 can have cold-like
symptoms, sore throat, brain fog, gastrointestinal problems, among many other
symptoms. We know now that a significant proportion of individuals with
COVID-19 remain symptomatic for months afterward. Their symptoms may wax and
wane leaving them devastated thinking things are finally getting better only to
be knocked down by persistent recurring fevers, fatigue, and heart palpitations
a month later. This virus can cause serious lung damage and we don't yet know
if people's lungs will fully recover or if they will have a lifetime of chronic
illness. Consider that several studies have put the percentage of so-called
"long COVID" at around 20-30% of cases. In the United States we've
had a little over 30 million documented cases. That translates to approximately 6-9
million people with long-term symptoms. Some of them may have permanent damage
to their lungs or heart. The devastation this virus is causing is immeasurable.
In the U.S.
approximately 15% of cases are hospitalized. Maybe you feel more tired and run
down than normal. You've got a fever and body aches; you have a cough and feel
a little sick to your stomach. Shortness of breath starts a week later, but you
try to soldier on. A few days after that you're in full blown respiratory
distress and being admitted to the hospital. If you make it out, you'll be
there for 10-13 days. Six percent of hospitalized patients are admitted to
the ICU. People can have strokes; their organs may start to fail.
Healthy, younger people
who become infected and don't get very sick spread the virus around. An
increase in cases leads to increased transmission. Hospitalizations and deaths
follow, primarily in the older population and those with underlying medical conditions like high blood pressure and diabetes. When
we look at hospitalizations by age, people aged 18-49 make up 30-40% of
hospitalized patients. This is not a benign illness that only seriously impacts
the elderly and you just don't know how your body is going to react to the infection.
How the vaccines work.
Now that we know what the virus looks like and how it can enter our body and infect our cells, let's learn about vaccines. Vaccines are a way to expose your body's immune system to a virus, bacterium, or parasite without you having to become infected and get sick. There are many ways that vaccines can do this. Each of the three COVID-19 vaccines currently available in the United States provide your immune cells with genetic information about how to make the spike proteins of SARS-CoV-2. Remember that the spike proteins are on the outer layer of the virus' coat and they are what allow it to attach to receptors on your cells and get inside. The vaccines differ in how that information gets to your immune cells.
The Moderna-NIAID and Pfizer-BioNTech vaccines are mRNA, or messenger RNA, vaccines. The mRNA in the vaccines is a blueprint for making a part of the spike protein of SARS-CoV-2. Remember that the spike protein is the part of the virus that attaches to ACE2 receptors on human cells. The mRNA in the vaccine only has information for making those spike protein parts, not for making the actual virus. Now, mRNA can’t travel around your body on its own, it would basically just disappear in a puff of smoke like the Wicked Witch. Or maybe it would fade away like Marty McFly does in that picture. Yes, I’m making old references. Yes, I’m old. Deal with it. Both the Moderna and Pfizer vaccines use a nanolipid to transport the mRNA around. Nanolipid is just a fancy way of saying teeny, tiny fat droplet. The nanolipid keeps the mRNA safe from being broken down by enzymes in your body and allows the mRNA to enter certain kinds of cells in the lymph nodes nearest the vaccination site. These cells are called antigen-presenting cells, or APCs. An antigen is a substance that is typically not found in the body and is, therefore, recognized by the immune system as something that needs to be removed, destroyed, or vanquished. See also my body's absolute panic at finding the same dust mite poop that it's always exposed to. "What is this???!!! We must get rid of it!! Fire the sneeze machine! Send it out in a waterfall from the face ports! Get it OUT!!!!" Or something like that, I imagine.
Once inside an APC called a dendritic cell, the nanolipid layer is broken down and the mRNA floats around in the cell cytoplasm until it runs into a ribosome. Sound familiar? Let's hold that thought and talk a little about the third vaccine.
The Johnson & Johnson-Janssen (J&J) vaccine uses a different delivery method than the nanolipid-mRNA system. It's called a viral vector, which means the genetic information needed to make the spike proteins is brought into your body by another virus. Scientists have done a bunch of science stuff to a virus called adenovirus type 26 to 1) make sure it won't make you sick and 2) give it the blueprints for making SARS-CoV-2 spike proteins. This time, the blueprints are added into the DNA of the adenovirus vector delivery system. Adenoviruses are common and cause illnesses such as colds, diarrhea, and pink eye. This particular one, type 26, is not commonly found in humans. This is important because it's highly unlikely that you have already been exposed to this adenovirus. If you had, and already have antibodies against it, your body would neutralize the virus vector and it would be unable to do its job. Again, highly unlikely. The adenovirus vector contains the information needed to produce SARS-CoV-2 spike proteins in its DNA. Once inside your body, the adenovirus binds to your cells, enters those cells, and releases the DNA. That DNA is then read and transcribed into mRNA by some of the nifty little gadgets inside of your cells. What happens next in terms of immune response is the same for all three vaccines.
We return to the show to
find our hero mRNA floating around the immune cell cytoplasm when suddenly it
bumps into a ribosome!
The ribosome reads the mRNA strand and makes the antigen
part of the spike protein. After that, the mRNA is broken down. Basically a
"burn after reading" spy situation. So now the dendritic
antigen-presenting cell (APC) has these spike protein antigens and it does two
things. 1) It presents the spike protein antigen by bringing it to its cell
surface so that it can be seen and 2) It sends the spike protein antigens out
of the cell using what's called the Golgi apparatus. The antigens presented on
the dendritic cell surface entice immune cells called cytotoxic T-cells to come
take a look. Think of a pie on a windowsill. A light breeze blows the scent of
flaky, buttery crust and warm apple and cinnamon right under the nose of a Yogi
Bear T-cell. The cytotoxic T-cells, also called CD8+ T-cells, are drawn over, bind to the substance that has presented the antigen on the dendritic
cell's surface, and then kill the cell. This is called cell-mediated immunity.
Cytotoxic T-cells go around the body looking for other cells with spike protein
antigens and kills them.
The spike protein
antigens that were shuttled out of the cell by the Golgi apparatus float around
until they are taken up by another type of APC called a macrophage. Once inside
the macrophage, the antigens are broken up and presented on its cell surface
using a slightly different substance than was used by the dendritic cells. This
substance entices a different kind of immune cell called a helper T-cell. These
T-cells, also called CD4+ T-cells, send out a signal to call over yet another kind
of immune cell called a B-cell. B-cells are the ones that create antibodies.
Therefore, this type of immune response is called antibody-mediated immunity.
The B-cells bind to the antigen and then split off into a clone of sorts called
a plasma cell with the aid of the helper T-cells. Plasma cells make a counter
substance to the antigen called an antibody, and they make a lot of them.
Millions of them, and rapidly. Antibodies bind to the antigens in such a way
that the spike proteins cannot then bind to your cell. The antibodies also mark
that cell for destruction. Artist's rendition poorly drawn by me.
All of this to say that
it's way more complicated than that and you could just watch this hilarious,
dramatic, and informative TikTok and go about your day. https://vm.tiktok.com/ZMekm5w83/
One more thing on
immunity. There are memory T-cells and memory B-cells that will remember the
spike protein antigen if ever encountered again. This allows for a faster, more
robust response.
A couple more things
about the vaccines. The mRNA from the Moderna and Pfizer vaccines does not enter the nucleus of your cells. The DNA from the J&J vaccine does enter the nucleus, but adenoviruses don't have the ability to integrate their DNA with the host. Neither the mRNA nor the DNA are able to change your genetic
code. Full stop. Nanolipids are not tiny pieces of technology that contain
microchips, they are just little tiny particles that don't dissolve in water
(like oil) and act as a protective coat around the mRNA.
But what about immunity from natural infection, isn't that better than from a vaccine? It is true the most robust immune response is going to be from becoming infected with SARS-CoV-2. Your body's immune cells go through the same processes recognizing antigens and making antibodies as they do because of the vaccine. However, what comes along with infection is disease, cell damage in your organs, long-term symptoms, and possibly hospitalization and death. Infections also lead to school closures, cancellation of concerts and sporting events, closed bars and restaurants, among many other consequences. The risks of infection far outweigh the risks of vaccination.
Let's talk side effects.
There are local side effects at the injection site. Most common are pain,
swelling, and redness. I would describe the pain as a deep bruise, but it
doesn't last for more than a few days. Less common but still totally normal is
itching and rash. Then there are side effects that you feel throughout your body.
These symptoms are related to your body doing the work of mounting an immune
response. Most common are body aches, tiredness, headache, fever, chills, and
nausea. You may have one or more of these symptoms and they may disrupt your life
for a day or two. From personal experience after my first Moderna shot, I had a
sore arm for a day or two. After the second shot, I had body aches, tiredness,
a barely elevated temperature, and my arm was more sore. The symptoms started
about 18-24 hours after the shot and were mostly gone later that night and the area around the injection site was just a little itchy. You'll be asked to wait 15 minutes after getting the shot before you leave just in case you have an allergic reaction. If you have had a severe allergic reaction to anything in the past, especially to any of vaccine components, be sure to tell the health care worker giving you the vaccine. They might ask that you wait 30 minutes.
You can find out if you're allergic to anything in the vaccine by checking out the ingredient lists which are publicly available on fact sheets.
 |
| https://twitter.com/atrupar/status/1338574124709507073 |
Pfizer: mRNA, lipids ((4-hydroxybutyl)azanediyl)bis(hexane-6,1-diyl)bis(2-hexyldecanoate), 2 [(polyethylene glycol)-2000]-N,N-ditetradecylacetamide, 1,2-Distearoyl-sn-glycero-3- phosphocholine, and cholesterol), potassium chloride, monobasic potassium phosphate, sodium chloride, dibasic sodium phosphate dihydrate, and sucrose.
Moderna: mRNA, lipids (SM-102, polyethylene glycol [PEG] 2000 dimyristoyl glycerol [DMG], cholesterol, and 1,2-distearoyl-sn-glycero-3-phosphocholine [DSPC]), tromethamine, tromethamine hydrochloride, acetic acid, sodium acetate, and sucrose.
Johnson & Johnson: adenovirus particles and the following inactive ingredients: citric acid monohydrate, trisodium citrate dihydrate, ethanol, 2-hydroxypropyl-β-cyclodextrin (HBCD), polysorbate-80, sodium chloride. Each dose may also contain residual amounts of host cell proteins and/or host cell DNA.
Don't be intimidated by all of the numbers and long words! For example, the chemical name of table salt, NaCl, is sodium chloride. Besides the mRNA for Pfizer and Moderna, and the virus particles for J&J the other ingredients are there to maintain a specific pH level and preserve the environment so that the active parts don't degrade and become useless.
Lipids: carry the mRNA; not water soluble; lubricant
Salts: potassium chloride, monobasic potassium phosphate, sodium chloride, sodium acetate, dibasic sodium phosphate dihydrate, trisodium citrate dihydrate
Sugar: sucrose
Acids: citric acid monohydrate, acetic acid
Acid stabilizers: tromethamine, tromethamine hydrochloride
Alcohol: ethanol
Emulsifier: polysorbate-80
Improves solubility: 2-hydroxypropyl-β-cyclodextrin (HBCD)
When you get vaccinated you can help keep track of side effects and help gain understanding of the vaccines' ability to protect against infection by participating in V-safe. V-safe is the CDC's smartphone-based after-vaccination health tracker. After you sign up, the tool will send you texts daily for a week after your vaccination asking about any symptoms you might be having. Then it sends a weekly text for 5 weeks asking about any symptoms and if you've had a positive COVID-19 test result. It will also send you a reminder for your second shot, if the vaccine you got the first time requires that. It's super easy and helps us all gain knowledge about the vaccines. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/vsafe.html
Each vaccine has a schedule too. The Pfizer vaccine is two shots 21 days apart; Moderna is two shots 28 days apart; J&J is one shot. These schedules are based on findings from the clinical trials for each vaccine, when the best immune response occurs.
Vaccine efficacy and variants.
If you've been paying attention to news media lately, you've been hearing a lot about viral variants and vaccine efficacy. What does it all mean?
Let's start with the variants. Every time the viral RNA is replicated, there is a chance that a change will occur. This change is called a mutation, and mutations occur all the time at random. A mutation can be just a single difference in the viral RNA strand. Remember that RNA is single strand of genetic information. On a closer level, the RNA strand is series of smaller segments called genes, which encode all of the parts that make a virion (spike, fat coat, RNA). What effect can a mutation have on the virus? Mutations can be beneficial, detrimental, or neutral. A change may make the virus more fit, less fit, or have no effect. Mutations are replicated and those that have a beneficial effect on the virus' structure make more virus with that mutation.
The variants that you've been hearing about in the news are classified as variants of concern, or VOCs. VOCs are so-called because the mutation or mutations that occurred have made that virus more fit. A mutation occurred that resulted in the spike protein having a higher affinity for the ACE2 receptor, meaning it can latch on more easily. The variant viral particles will be able to infect more of your body's cells and replicate so that there will be higher numbers of the variant than of the wild type. As you breathe, talk, sing, cough, or sneeze you will be expelling more of the variant virus. That's how the variants can become the dominant strain in your body and in the community. And the more virus circulating around, the more likely we are to encounter variants. If someone who has been vaccinated becomes infected, the virus in their body is likely to mutate in order to avoid being tagged by antibodies. Survival of the fittest and all that. While the virus is widely circulating, we're asking that people who are vaccinated continue to wear masks and maintain social distance in part to reduce the chances of creating even more variants.
All the available COVID-19 vaccines have advantages and disadvantages, and they all have varying levels of
efficacy. We can't directly compare any of the vaccines to each
other to determine which is "best" or most effective. There are too
many factors that differ; from the delivery methods to when the research trials
occurred to what the primary endpoints of the trails were. Endpoints are the
outcomes or goals of research trials. Primary endpoints varied. For example, one manufacturer's primary endpoint was protection of
symptomatic infection 7 days after second dose and another's was protection against
moderate to severe infection at 14 and 28 days after one dose. These goals are
similar, but different enough so that we can't directly compare the results to each
other. Some vaccine manufacturers had completed research trials before the emergence
of virus variants that have differences in the spike protein. If the vaccine
contains information to make a specific version of the spike protein, how well
does it protect against a virus with a slightly different spike?
Emergency use authorization and vaccine safety.
You may have concerns about getting a COVID-19 vaccine because they have not been fully approved by the Food and Drug Administration (FDA) here in the U.S., or whichever group approves vaccines in your country. Completely understandable. Let's talk about emergency use authorization, or EUA. Emergency use authorization allows the FDA to preliminarily approve a medical device, medication, laboratory test, or vaccine for use to diagnose, treat, or prevent a life-threatening disease or condition. EUA can be given during public health emergencies and in situations of compassionate care. The product must meet a set of stringent criteria before an EUA may be given. This page on the FDA website gives a more in-depth explanation of the process. https://www.fda.gov/vaccines-blood-biologics/vaccines/emergency-use-authorization-vaccines-explained
The vaccine manufacturers with EUA for their vaccines have been able to show that the benefits of the vaccine outweigh any known or possible risks and that the primary endpoints of preventing severe disease and death from COVID-19 are met. The vaccines have been shown to be safe and effective and there is an expectation from FDA that the manufacturers continue to monitor trial participants.
I wanted to understand more about how we have vaccines available in less than one year when normally it can take many years to get a vaccine from concept to approval. Turns out there are a lot of factors involved, not the least of which are collaboration, use of previous knowledge and technology, and money. Researchers can spend a long time in what's called the preclinical phase pouring over journal articles, experimenting with the virus to learn about its parts, and trying out different combinations to induce immune response in mice or other research animals. That's just to figure out the best possible options for the vaccine and it can take years. In the case of SARS-CoV-2, researchers from all over the world worked together to map out the virus and all its various parts and to determine the best potentials for vaccines. Another time-consuming part of the vaccine development process is finding the right delivery method and dose. Research into adenovirus vector technology has been ongoing for decades and J&J had already used adenovirus type 26 in its successful Ebola vaccine. The Pfizer and Moderna vaccines are the first of their kind, but research into using mRNA in vaccines started 30 years ago. Researchers had already done most of the heavy lifting when SARS-CoV-2 came onto the scene. The U.S. government gave a lot of money to pharmaceutical companies to pay for the research. When researchers don't have to spend the majority of their time writing grant proposals and worrying about how to keep the lights on, they are better able to do the actual sciencing.
The vaccine trial process was also accelerated by combining trial phases that would under normal circumstances be separate. This allowed for checking vaccine safety and efficacy outcomes in parallel rather than sequentially. The manufacturers also enrolled more people in their phase 3 trials in order to have a more robust study. More people in the study means there is increased likelihood of finding adverse events and also increases the power of the study to find differences between the vaccine group and the placebo group.
I found these two articles to be informative and easy to understand.
https://news.uchicago.edu/story/how-were-researchers-able-develop-covid-19-vaccines-so-quickly
We've cut down on the research time by years, and we have large groups of vaccinated people being studied. So, what are we missing? Follow-up time. How long does immunity last and how often will we need to be vaccinated? Transmissibility. If I'm vaccinated can I still spread the virus to others? Safety and efficacy among different groups. Pregnant people and children are participating in vaccine trials right now because they weren't included in the initial phase 3 studies. Efficacy of the vaccines against VOCs. Moderna and Pfizer clinical trials occurred prior to the emergence of variants. New variants have emerged since J&J and others went through their clinical trials. Each manufacturer is testing their vaccines against VOCs to determine if they still work and labs around the world are testing people who have been vaccinated to find so-called breakthrough infections. What we're doing in the lab is taking samples from vaccinated people who are SARS-CoV-2 positive and checking out that virus. By looking at the RNA strand of the virus, we can figure out if the person was infected by a variant that has changed enough to evade the antibodies created in response to the vaccine. If we start seeing that and a lot of it, vaccine manufacturers will have to go back to the drawing board, and you and I may need to get a booster shot to protect against that variant.
There is no vaccine in existence that prevents you from being exposed to a microbe that can make you sick. They don't create an invisible barrier around your body. And there are no vaccines that are 100% effective at preventing COVID-19, so there will be fully vaccinated people who still get sick. However, the vaccines are extremely effective at preventing death and disease severe enough to require hospitalization. Early studies are showing that they can prevent most symptomatic illness. And a recent release in the Morbidity and Mortality Weekly Report shows some very promising results. Fully vaccinated health care workers, first responders, and other essential and frontline workers were 90% less likely to be infected with SARS-CoV-2 than their unvaccinated counterparts. The study participants had received Pfizer or Moderna mRNA vaccines. This study shows evidence that vaccination can prevent infection, not just moderate to severe disease. https://www.cdc.gov/mmwr/volumes/70/wr/mm7013e3.htm?s_cid=mm7013e3_w
But we need to get as many people vaccinated as possible as quickly as we can in order to get there. Otherwise, the virus will still be transmitting, replicating and mutating, and making people sick. Many places in the U.S. have loosened restrictions and we're now seeing case counts on the rise again after a brief plateau. https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases
How high the rise goes is up to us. Do your part by getting vaccinated when it's your turn. Until then keep wearing your masks, stay home if you are able, wash your hands frequently, get tested if you've been exposed or you feel sick, and answer the phone when contact tracers call you.
There is a ton of misinformation and disinformation out there about COVID-19, the vaccines, masks, and pretty much anything related to this pandemic. I urge you to be skeptical of anything that you read on social media and even some news outlets. Except me. You can trust me.
One year after the pandemic was declared by the World Health Organization, there are several vaccines being administered worldwide. Millions of people are now protected from getting extremely sick and needing to be hospitalized. Millions of people's lives will be saved. That is absolutely amazing, and we should celebrate!
 |
| https://tenor.com/bumB2.gif |